Amniocentesis is a medical procedure used to diagnose certain genetic abnormalities in the fetus during pregnancy. This prenatal test provides important information about the baby’s health and may be recommended in specific situations.
For many years, the word amniocentesis has been a source of fear for many pregnant women, but let’s get to know this procedure better and consider all aspects together.
What is amniocentesis?
Amniocentesis is a so-called “invasive” prenatal test that provides crucial information about your baby’s health by taking a sample of amniotic fluid (the fluid in which your baby floats). The most common reason a woman requests an amniocentesis or why it’s prescribed by a gynecologist is to rule out the presence of chromosomal disorders or genetic abnormalities, such as Down syndrome, for example. Both amniocentesis and chorionic villus sampling (another invasive prenatal test) serve this diagnostic purpose.
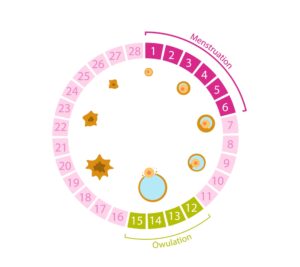
Amniocentesis is typically performed between the 15th and 18th week and allows for the determination of the fetus’s karyotype, in simple terms, you can have a detailed map of your baby’s genetic heritage.
How is it performed?
Amniocentesis should always be performed by a gynecologist, and the more experienced they are, the less painful the procedure will be.
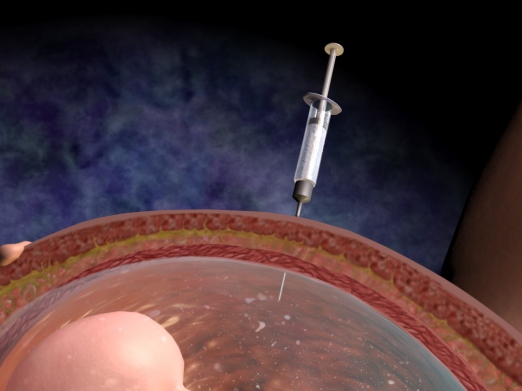
The amniotic fluid is the fluid composed of fetal exudates and urine that fills the uterine cavity. This fluid contains amniocytes, which are fetal shedding cells used to replicate the baby’s genetic heritage.
The quick (lasting about 1 minute) sample is taken through the transabdominal route, always under ultrasound guidance, using a needle to draw the fluid directly from the maternal uterus. Before proceeding with this test, however, the operator must ensure certain conditions:
- Fetal vitality (to be checked at the beginning and end of the sampling).
- Gestational age
- Fetal location
- Exclusion of multiple pregnancies
- Placental location
- Amount of fluid
- Depth of the layer
Once sure that a sufficiently large layer (small layers or those near the placenta or fetal head should be excluded) has been found from which to draw the fluid, the needle will be inserted, and approximately 15-20 ml of fluid will be aspirated.
The position the mother should assume is supine, and there is no need for any anesthesia. In fact, if your gynecologist has skilled and precise hands, you won’t feel any pain.
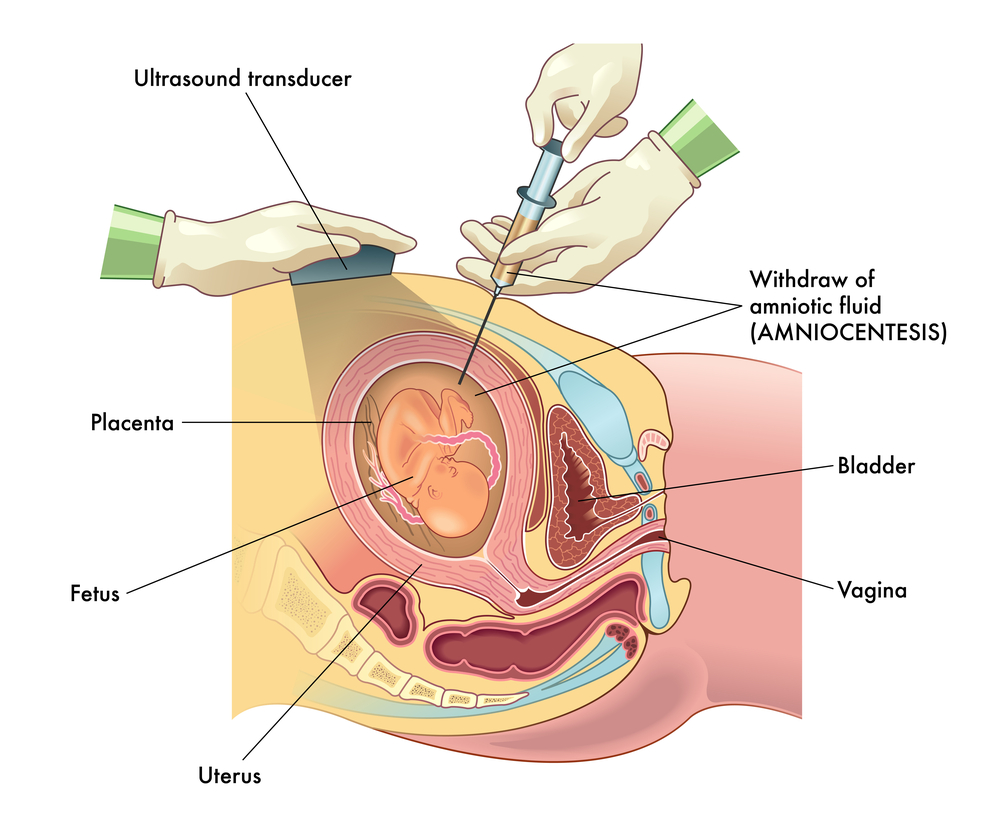
After taking your position, the healthcare providers will disinfect your skin from the navel to the pubic area, delineating the area with sterile drapes. The doctor, always in a sterile manner and under ultrasound guidance, will direct the thin needle into the uterine cavity through the transabdominal route. The ultrasound guidance is used to guide the path of the needle without causing harm to the fetus or its attachments (placenta and umbilical cord). Once in the amniotic pool and the fluid sample is collected, it will be sent to the cytogenetic laboratory for analysis.
After the procedure, it’s advisable for the mother to rest for at least two days, trying to avoid exertion and fatigue. If you experience cramps, contractions, or any bleeding or amniotic fluid leakage, you should immediately contact your doctor.
The turnaround time for the test results is approximately 20 days.
Who is amniocentesis recommended for?
Amniocentesis is a test that your doctor cannot impose on you because it’s a choice for the parents, but they may strongly recommend it if:
- The mother is at least 35 years old
- One or both parents have genetic mutations or chromosomal alterations
- There is at least one case of aneuploidy in the family
- Chorionic villus sampling has shown mosaicism
- There is doubt about fetal malformations (nuchal translucency) based on the ultrasound examination
- The result of a bi-test or tri-test is positive
In public healthcare facilities, the test is free for women who are 35 years of age or older, as well as for those with a confirmed risk of developing chromosomal disorders. In private facilities, the cost is typically between €1,000 and €1,500.
What risks do I face when undergoing amniocentesis?
Is amniocentesis dangerous? It’s a question that many pregnant women ask.
Women often fear amniocentesis due to the risk of miscarriage, although it’s extremely low and has been attributed to it in the past thirty years. According to recent research, however, there are no differences in the incidence of spontaneous abortion, stillbirth, and prenatal mortality between women who have undergone amniocentesis and those who have not. The risk of miscarriage is very low, representing 0.031%; nevertheless, the operator must be capable of performing this procedure to eliminate any risk, as the success of the test largely depends on the professionalism and skills of the doctor.
Amniocentesis is considered a relatively safe procedure, but like any medical intervention, it carries some risks. However, it’s important to note that these risks are generally low, and the doctor will take all necessary precautions to minimize them. If you have concerns or questions about specific risks, consult your doctor.
When is amniocentesis performed?
In what situations is amniocentesis recommended?
Amniocentesis is typically recommended when there is an increased risk of genetic abnormalities in the fetus. Situations in which it may be recommended include:
- Advanced maternal age: Women over the age of 35 have a slightly higher risk of having a baby with genetic abnormalities, such as Down syndrome. Therefore, amniocentesis may be suggested as part of prenatal monitoring.
- Abnormal screening results: Prenatal screening tests, such as first-trimester screening or second-trimester screening, can detect possible fetal abnormalities. If the results of these tests are abnormal, amniocentesis may be recommended to confirm the diagnosis.
- Family history of genetic abnormalities: If there is a family history of inherited genetic abnormalities or congenital diseases in the mother’s or father’s family, amniocentesis may be recommended to check for the presence of these conditions in the fetus.
When not to have amniocentesis?
Situations in which amniocentesis may not be recommended include
Despite its benefits, there are some situations in which amniocentesis may not be recommended or may be considered an individual choice. These include:
- Low-risk pregnancy: If a woman is young and healthy, with no family history of genetic abnormalities and with normal prenatal screening results, amniocentesis may not be necessary. However, it’s important to discuss with the doctor to assess the risks and benefits based on the specific situation.
- Personal preferences: Some women may choose not to undergo amniocentesis due to the risk of miscarriage associated with the procedure. It’s important for each woman to make an informed decision based on her own circumstances, consulting with the doctor and carefully considering the potential risks and benefits.
Is amniocentesis mandatory?
Amniocentesis is not mandatory during pregnancy. It is a choice made based on individual circumstances and the personal preferences of the woman. However, if there are risk factors or specific medical indications, the doctor may recommend amniocentesis as part of prenatal monitoring.
Is amniocentesis painful?
During amniocentesis, a needle is inserted through the abdominal wall into the uterine cavity to collect a sample of the amniotic fluid surrounding the fetus. The procedure can cause a sensation of pressure or cramping similar to menstrual cramps. Some women may experience mild discomfort, but most doctors use local anesthesia to minimize pain. It’s important to communicate with the doctor during the procedure to ensure maximum comfort.
What is the ideal week for amniocentesis?
Amniocentesis is typically performed between the 15th and 20th week of pregnancy. This timeframe provides an adequate window for diagnosing genetic anomalies in the fetus. However, in certain specific circumstances, amniocentesis may be performed after the 20th week if necessary. The doctor will evaluate the individual situation and provide specific information about timing.

 Italiano
Italiano